Are you considering getting a bone graft? Whether you’re planning for a dental implant, orthopedic surgery, or dealing with bone loss, it’s important to have all the essential information.
In this comprehensive guide to bone grafts, we will cover everything you need to know. From explaining what bone grafts are and why they are necessary, to discussing the different types of bone grafts available and how the procedure works, we will leave no stone unturned.
Our aim is to provide you with a clear understanding of bone grafts, their benefits, risks, and potential complications. We will also explore the recovery process and offer tips on how to maximize the success of your bone graft.
Whether you’re a patient seeking more knowledge or a healthcare professional looking to enhance your expertise, this guide will serve as your go-to resource for all things bone grafts. So, let’s dive in and unravel the mysteries of bone grafting together.
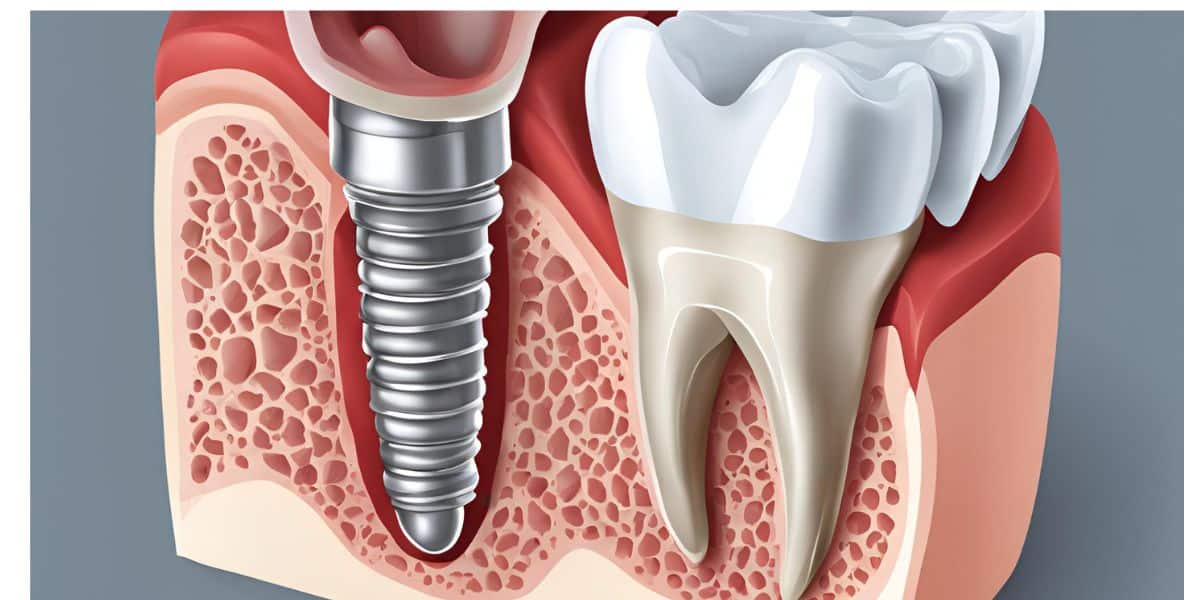
Table of Content
Key Takeaways
- Purpose and Function: A bone graft is a surgical procedure that transplants bone tissue to repair a damaged area. Its main purpose is to provide a “scaffold” that encourages the body to grow new, healthy bone.
- Types of Grafts: There are three primary sources for bone grafts: autografts (bone from the patient’s own body, often considered the “gold standard”), allografts (bone from a human donor), and synthetic grafts (man-made, biocompatible materials).
- Success and Risk Factors: While success rates can be high, the healing process is long (often several months). The risk of complications or graft failure is significantly increased by factors such as smoking, periodontal disease, osteoporosis, and uncontrolled systemic conditions like diabetes.
What is a bone graft?
A bone graft is a dental surgical procedure that involves the transplantation of bone tissue to repair or rebuild bones that have been damaged due to injury, disease, or surgical procedures.
The primary purpose of a bone graft is to provide a scaffold for new bone growth, facilitating the healing process and restoring the structural integrity of the affected area. It can be utilized in various medical fields, including dentistry, orthopedics, and spinal surgery, depending on the specific needs of the patient.
Bone grafts can be classified into various categories based on their source and composition. They may be harvested from the patient’s own body, known as autografts, or obtained from a donor, called allografts. Synthetic materials, or bone graft substitutes, can also be used to promote bone healing. Regardless of the type, the goal remains the same: to stimulate new bone formation and ensure that the skeletal system can function optimally.
Understanding the concept of bone grafting is crucial for anyone considering this procedure. It not only sheds light on the mechanics of how bone healing occurs but also emphasizes its significance in restoring health and functionality. With a solid grasp of what bone grafts are, patients can better navigate the process and make informed decisions concerning their treatment options.
Reasons for needing a bone graft
There are several reasons why a patient might require a bone graft. One of the most common reasons is to support dental implants. In cases where there has been significant bone loss in the jaw, a bone graft can provide the necessary foundation for the implant to be securely placed. This is particularly crucial for individuals who have suffered from tooth loss due to decay, periodontal disease, or trauma, as the absence of adequate bone can jeopardize the success of the implant.
Another prevalent reason for a bone graft is to repair fractures that have not healed properly, a condition known as nonunion or malunion. In such cases, a bone graft can assist in bridging the gap between the broken ends of the bone and stimulate healing, promoting new bone growth. This can be especially important for fractures in areas with limited blood supply or in patients with underlying health issues that impede healing.
Additionally, bone grafts are often necessary in orthopedic surgeries to reconstruct damaged joints or bones, such as in cases of arthritis or severe bone loss due to tumors. These surgeries aim to restore function and relieve pain, making bone grafting an essential component of the treatment process. Whether for dental, orthopedic, or reconstructive purposes, the need for bone grafts is often driven by the goal of restoring normal anatomy and functionality.
Types of bone grafts
Bone grafts can be categorized into different types based on their source and material composition. The three primary types are autografts, allografts, and synthetic grafts 1.
- Autografts: involve harvesting bone from the patient’s own body, typically from areas like the hip, wrist, or leg. This type is often considered the gold standard since it contains living cells and growth factors that enhance healing and integration with the surrounding bone.
- Allografts: on the other hand, are sourced from deceased donors and are processed to ensure safety and sterility. They are widely used because they eliminate the need for an additional surgical site for the patient. Allografts can be particularly beneficial for larger grafts or in patients who may not be suitable candidates for autografting due to other health concerns. The use of allografts, while safe, does require careful screening to reduce the risk of disease transmission.
- Synthetic grafts: also known as bone graft substitutes, are made from biocompatible materials such as synthetic hydroxyapatite (HA), Tricalcium phosphate (TCP), ceramics, calcium sulfate, metals or polymers . These materials are designed to mimic the properties of natural bone and provide a scaffold for new bone growth. Synthetic grafts can offer advantages such as reduced risk of infection and no need for donor tissue. However, they may not always integrate as effectively as autografts or allografts.
Understanding these differences is critical for patients and healthcare providers to determine the most suitable option based on individual circumstances and treatment goals.

Bone grafting procedure
The bone grafting procedure typically begins with a thorough evaluation by a healthcare provider to determine the appropriate type of graft and plan for the surgery. This may involve imaging studies such as X-rays or CT scans to assess the condition of the bone and the extent of the required grafting. Once the planning is complete, the patient is prepared for surgery, which is usually performed under local anesthesia, sedation, or general anesthesia, depending on the complexity of the procedure.
During the procedure, the surgeon will make an incision to access the affected area and prepare the site for graft placement. If an autograft is being used, the surgeon will harvest bone from another part of the patient’s body.
After preparing the bone graft, it is carefully placed in the targeted area, ensuring that it is securely positioned to promote optimal healing.
The surgeon then closes the incision with sutures or staples, and the area is bandaged to protect it during the initial recovery phase.
Post-operative care is crucial for the success of the bone graft. Patients are often given specific instructions regarding pain management, activity restrictions, and signs of complications to watch for.
Follow-up appointments are scheduled to monitor the healing process and ensure that the graft is integrating successfully with the existing bone.
Understanding the steps involved in the bone grafting procedure can help alleviate patient anxiety and prepare them for what to expect during recovery.
Recovery and healing process
The recovery process following a bone graft can vary depending on the individual’s health, the type of graft used, and the specific procedure performed.
Generally, patients can expect some swelling, discomfort, and bruising around the surgical site, which can last for several days to weeks. Pain management is often achieved through prescribed medications, and it’s essential for patients to follow their healthcare provider’s recommendations closely.
During the initial recovery phase, patients are typically advised to limit physical activity to allow the graft to stabilize and integrate with the surrounding bone.
Weight-bearing restrictions may be imposed, particularly if the graft is in a weight-bearing area such as the leg or spine. Adhering to these restrictions is critical in preventing complications and ensuring that the graft heals properly. Patients should also maintain a balanced diet rich in nutrients that support bone healing, such as calcium and vitamin D.
As the healing process progresses, patients will have follow-up appointments to assess bone integration, remove stitches and monitor for any potential complications.
Imaging studies, usually x-rays may be performed to evaluate the success of the graft.
Full recovery can take several months, and patients should remain patient during this time in order to the bone to regenerate.
Risks and complications of bone grafts
Like any surgical procedure, bone grafting carries certain risks and potential complications that patients should be aware of before undergoing the procedure.
One of the primary concerns is the possibility of infection at the surgical site, which can occur if bacteria enter the wound. Proper post-operative care and hygiene are crucial in minimizing this risk, and patients should be vigilant for signs of inflammation, increased pain, or discharge from the incision.
Another concern is the possibility of graft failure, wherein the graft does not properly integrate with the existing bone or heal as intended. This can happen due to various factors, including inadequate blood supply, underlying health conditions, or non-compliance with post-operative instructions. In some cases, a failed graft may require additional surgery to address the issue, leading to extended recovery times and increased healthcare costs.
Additionally, patients may experience complications related to harvesting an autograft, such as pain or complications at the donor site. It’s essential for patients to discuss any pre-existing health conditions or medications that could impact healing with their healthcare provider.
Factors that can increase the risk of bone graft failures
Studies have shown the following as the main risk factors for bone grafts failures: 2
- Periodontal disease
- Smoking
- Osteoporosis
- Surgical errors
- Systemic conditions such as uncontrolled diabetes
- Immune system deficiencies
Understanding these risks can empower patients to make informed decisions and engage in proactive measures to ensure the best possible outcome from their bone grafting procedure.
Bone graft success rates
The success rates of bone grafts can vary significantly depending on multiple factors, including the type of graft used, the patient’s overall health, and the specific location and condition of the bone being treated.
Generally, autografts are considered to have the highest success rates due to their compatibility and biological properties that promote healing. Studies have shown that autografts can achieve success rates exceeding 90% in many cases, making them a reliable option for various applications.3
Allografts also demonstrate favorable success rates, although they may be slightly lower than those of autografts. The success of allografts can depend on factors such as the quality of the donor tissue and the surgical technique employed. In many instances, allografts have been shown to achieve success rates between 70% and 90%, making them a viable alternative for patients who may not be candidates for autografting.
Synthetic grafts exhibit variable success rates, often influenced by the specific material used and the individual patient’s healing response. While some synthetic materials have been shown to perform well, others may not integrate as effectively with natural bone, leading to lower success rates.
Studies show no significant differencen among the type of bone graft used 4 so synthetic bone substitutes or xenologous bone grafts can be used as an alternative to autologous graft in order to overcome problems of additional surgeries or limited graft availability.
Overall, discussing expectations and success rates with a healthcare provider can help patients make informed choices regarding their treatment options and understand the likelihood of a favorable outcome.
Alternatives to bone grafts
For patients who may not be suitable candidates for traditional bone grafting or who wish to explore alternative options, there are several alternatives available.
One alternative is the use of growth factors and stem cell therapy. These advanced techniques aim to enhance the body’s natural healing processes by introducing specific proteins or stem cells that promote bone regeneration. While still relatively new, these methods show promise in certain clinical situations and may reduce the need for traditional grafting techniques.
Additionally, some patients may benefit from less invasive procedures, such as guided bone regeneration or distraction osteogenesis, which aim to enhance bone growth without the need for grafting. These alternatives can provide viable options for patients seeking to avoid the risks and complications associated with traditional bone grafting.
It is essential for patients to consult with their healthcare providers to determine the most appropriate treatment plan based on their unique circumstances and medical history.
Cost of bone grafts
The cost of bone grafts can vary widely depending on several factors, including the type of graft used, the complexity of the procedure, and the geographic location of the surgical facility.
Autografts tend to be more expensive due to the need for an additional surgical site to harvest the bone. This added complexity and the associated anesthesia and recovery costs can significantly influence the overall expense.
Allografts may be more cost-effective since they eliminate the need for a second surgical site, but they can still be pricey due to processing and storage fees associated with donor tissue.
Synthetic grafts might offer a more affordable option in some cases; however, the cost can vary depending on the materials used and the specific application.
Insurance coverage can also play a significant role in determining out-of-pocket costs for patients. Many insurance plans may cover a portion of the expenses associated with bone grafting, but coverage can differ based on the specific procedure and the patient’s medical history.
Patients should consult with their insurance providers and healthcare teams to obtain a clearer understanding of potential costs and coverage options before proceeding with treatment.
Conclusion
In conclusion, bone grafts are a critical component of modern medicine, offering solutions for various conditions related to bone loss and injury.
Understanding the intricacies of bone grafting, including the types available, reasons for their use, and the associated risks and benefits, is essential for making informed decisions regarding treatment. With advancements in technology and techniques, patients can expect improved outcomes and a better quality of life following bone graft procedures.
The recovery process, while requiring patience and diligence, is an opportunity for patients to engage in their health journey actively. By following medical advice and participating in rehabilitation, individuals can maximize the success of their grafts and restore their functionality.
As research continues to evolve, exploring alternatives and innovations in bone grafting will further enhance the options available to patients. Ultimately, working closely with healthcare providers to understand the specifics of one’s condition and treatment plan can lead to successful outcomes and improved health. Whether navigating the complexities of a dental implant or recovering from orthopedic surgery, knowledge is a powerful tool in the journey toward healing.
References
- Sandleen Feroz, Peter Cathro, Sašo Ivanovski, Nawshad Muhammad, Biomimetic bone grafts and substitutes: A review of recent advancements and applications,
Biomedical Engineering Advances, Volume 6, 2023, 100107, ISSN 2667-0992, https://doi.org/10.1016/j.bea.2023.100107. ↩︎ - Elakkiya S, Ramesh AS, Prabhu K. Systematic analysis on the efficacy of bone enhancement methods used for success in dental implants. J Indian Prosthodont Soc. 2017 Jul-Sep;17(3):219-225. doi: 10.4103/jips.jips_19_17. PMID: 28936034; PMCID: PMC5601489. ↩︎
- Elakkiya S, Ramesh AS, Prabhu K. Systematic analysis on the efficacy of bone enhancement methods used for success in dental implants. J Indian Prosthodont Soc. 2017 Jul-Sep;17(3):219-225. doi: 10.4103/jips.jips_19_17. PMID: 28936034; PMCID: PMC5601489 ↩︎
- Spyridon N. Papageorgiou, Panagiotis N. Papageorgiou, James Deschner, Werner Götz,Comparative effectiveness of natural and synthetic bone grafts in oral and maxillofacial surgery prior to insertion of dental implants: Systematic review and network meta-analysis of parallel and cluster randomized controlled trials, Journal of Dentistry, Volume 48, 2016, Pages 1-8, ISSN 0300-5712, https://doi.org/10.1016/j.jdent.2016.03.010. ↩︎





